In order to understand the connection between eating disorders and trauma, it is helpful to first understand the function of the eating disorder. For some individuals, eating disorder behaviors become an unhealthy way of coping with stressors that are out of an individual’s realm of control. Trauma can be one of these stressors. While the eating disorder can help individuals to avoid or escape uncomfortable feelings in the moment, in the long term, using maladaptive eating disorder behaviors to cope will most often increase distress, preventing independence, growth and/or self-efficacy.
In order to understand the connection between eating disorders and trauma, it is helpful to first understand the function of the eating disorder. For some individuals, eating disorder behaviors become an unhealthy way of coping with stressors that are out of an individual’s realm of control. Trauma can be one of these stressors. While the eating disorder can help individuals to avoid or escape uncomfortable feelings in the moment, in the long term, using maladaptive eating disorder behaviors to cope will most often increase distress, preventing independence, growth and/or self-efficacy.
Trauma is a life experience that involves actual or perceived threats to the safety and well-being of an individual or someone close to that individual. Traumatic events overwhelm a person’s mind and body and cause extreme emotional, psychological and physiological distress. Post-traumatic stress disorder (PTSD) is the correlating diagnosis for trauma which identifies symptoms resulting from trauma events. These symptoms can include flashbacks, dissociation, hyper-vigilance, mistrust, exaggerated startle response and disrupted sleep.
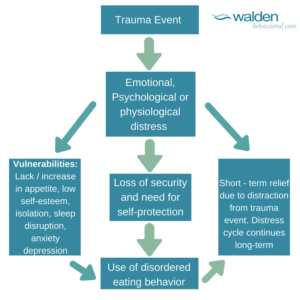
Now that we understand eating disorders and trauma , let’s examine how the two can correlate. The diagram below can help delineate what can often be a causal relationship. I think that it is important to note that individuals responding to trauma with eating disorder behaviors begin experiencing amplified emotional, psychological and physiological distress, thus reinforcing the need to continue the use of behaviors over time. Individuals can get stuck in this problem cycle even after the trauma event has passed.
At Walden Behavioral Care we treat eating disorders including but not limited to anorexia, bulimia, and binge-eating disorder, and co-occurring PTSD diagnoses through the practice of trauma-informed care. Research studies have identified that 3 out of 10 individuals with eating disorders have suffered trauma, specifically childhood sexual abuse. It is common through eating disorder recovery to see that decreasing eating disorder symptoms can trigger a rise in PTSD symptoms (and vice versa). In establishing a safe space to slow down their thoughts and emotions, individuals are better able to gain insight into the relationship between their trauma and their eating disorder\. Working on the eating disorder, with an increase in understanding of their individual trauma maximizes the effectiveness of skills. Evidence – based treatments such as cognitive behavioral therapy and dialectical behavioral therapy teach emotion regulation, ability to express thoughts and emotions and impulse management. Through recovery, clients learn about their vulnerabilities and are better equipped to meet their basic needs, including consistent nourishment. Through our person -centered approach, we remind individuals of their empowering resilience.
“The human spirit is stronger than anything that can happen to it.” (C.C. Scott)
If you are having a difficult time dealing with a concurrent trauma and an eating disorder, we can help.
####
Allison Lara, LMFT, is an adult clinician at the Peabody Clinic, providing therapy to clients participating in the partial hospitalization program and intensive outpatient program. Allison received her Bachelor’s Degree in Psychology from Providence College, and her Master’s Degree in Marriage & Family Therapy from Seton Hall University. Allison has been a practicing therapist since 2011 and has worked in NY, NJ and MA. Allison works with clients using a solution focused approach and implements CBT and DBT interventions. Allison has been facilitating a trauma breakout group for clients to focus on developing skills to contain emotions and thoughts related to trauma events. Allison also has a post-graduate certificate in fine arts and enjoys creating artwork.